
— OPINION —
In what has become a far too common and troubling occurrence, another whole genome sequenced (WGS) patient — one of the 61 confirmed sick in June 2024 — has come forward long after the outbreak was deemed over and without the benefit of being told by health authorities that he in fact was a victim linked to the outbreak.
Let’s put this into perspective. Once someone is sick enough to seek medical treatment and test positive for Listeria in either blood or spinal fluid, that hospital lab is under a legal obligation to contact health officials who will then reach out to the victim or the surviving family (more on that in a bit) and the Listeria isolate sent to the state lab for genetic testing. Once completed, the test is uploaded to the CDC’s PulseNet to compare to other clinical, product and/or environmental samples — that is how we got to 61 ill.
At the same time local and/or state health officials are gathering not only the victim’s bodily fluids, but completing detailed questionnaires and collecting a food history (Listeria has an incubation period of 3-70 days), shopper card and debit and credit card card receipts. All with the admirable goal of figuring out the outbreak cause and preventing more illnesses — and, learning how the outbreak happened to try and prevent the next one.
However, once the victim’s link is confirmed and the cause of the outbreak isolated, it is becoming more and more common to learn that the victim or victim’s family is never told by health officials the cause of the illness or the victim’s link to a confirmed outbreak and source.
The latest call I took was because the victim read about my work in the paper and wondered if I could help him find the cause of his Listeria illness. Well, I have.
Question, why does public health not do the same?

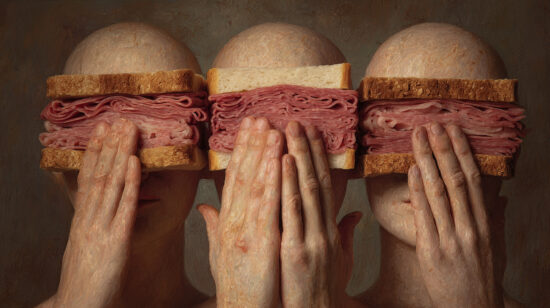
On July 12, 2024, the USDA’s Food Safety and Inspection Service (FSIS) launched an investigation into a multistate outbreak of listeriosis linked to retail-sliced deli meats. The investigation was triggered when the Maryland Department of Health detected Listeria monocytogenes in a sample of liverwurst. In response, the Maryland Department of Health, in collaboration with the Baltimore City Health Department, collected additional unopened liverwurst products from a retail store for testing. Subsequent testing confirmed that these samples were also contaminated with the outbreak strain of Listeria monocytogenes, as identified through whole genome sequencing (WGS).
The USDA’s traceback investigation, done in conjunction with the Centers for Disease Control and Prevention and state public health partners, narrowed the source of the outbreak to Boar’s Head’s Jarratt, VA, plant. Epidemiologic, laboratory, and traceback data showed that meats sliced at deli counters, including Boar’s Head brand liverwurst, were contaminated with Listeria and were responsible for making people ill.
In response to the outbreak, Boar’s Head issued a recall for some of its deli meat products, including liverwurst, on July 26, 2024. The recall was expanded on July 30, 2024, to include an additional 7 million pounds of ready-to-eat (RTE) meat and poultry products.
This expanded recall affected 71 products produced between May 10, 2024, and July 29, 2024, under defendant’s Boar’s Head and Old Country brand names. The affected products included both deli-sliced meats and pre-packaged meat and poultry products. These products, bearing “sell by” dates ranging from July 29, 2024, through October 17, 2024, were distributed to retail locations across the U.S., with some exported to the Cayman Islands, Dominican Republic, Mexico and Panama. The products involved in the recall were identified by the establishment number “EST. 12612” or “P-12612” inside the USDA mark of inspection on the product labels.
On July 31, 2024, FSIS suspended all production at Boar’s Head’s Jarratt, Virginia plant. By mid-September 2024, Boar’s Head announced the indefinite closure of the Jarratt facility, which had been identified as the source of the deadly outbreak, and the permanent cessation of all liverwurst production.
(To sign up for a free subscription to Food Safety News, click here)